A new horizon for reproductive health and healthy ageing
Ovarian rejuvenation is not just about conception — it’s about restoring ovarian function at every stage of life. Whether due to natural aging, premature ovarian decline, or other causes, our innovative SEGOVA method offers new hope to improve reproductive potential and overall well-being.
With SEGOVA, you are choosing a method based on advanced biotechnology using only your body’s natural resources: your own cells and growth factors.
Main goals of the program:
- Improve reproductive potential at any age.
- Prolong ovarian function and hormonal balance.
- Support healthy ageing and longevity.
Ovarian rejuvenation is an innovative procedure that is giving new hope for women around the world suffering from difficulties in conceiving and getting pregnant. Infertility treatments and ovarian rejuvenation are difficult for us to think about because the whole concept is fraught with uncertainties and unknowns. Even successful treatments are sometimes met with skepticism if only because there is too much incorrect information in circulation.
The good news is that many women who have chosen ovarian rejuvenation have actually had very positive results, and the outcomes are well documented and point to a much-improved success rate among women who have had no results using more traditional methods. As we will see further on, ovarian rejuvenation is all about stimulating natural processes in the ovaries and, as such, is much more conducive to success.
But what exactly is ovarian rejuvenation, and how does it work in practical terms? This is precisely what we will look into here, and it will be easy to see why so much is being written about this next level of fertility treatment and its promise to women all over the world.
With advances in medical treatments such as ovarian rejuvenation and work with stem cells and Platelet-Rich Plasma (PRP) by reputable laboratories such as SEGOVA Biotechnology, it is conceivable that we shall one day soon consider infertility no longer to be a problem.
What is ovarian rejuvenation?
Simply stated, ovarian rejuvenation is a process whereby the ovaries are stimulated to induce follicle growth and produce eggs for fertilization. It is a procedure that creates new eggs in the ovaries of women who may be unable to conceive for various reasons, such as more advanced maternal age, early menopause, or a low egg (oocyte) reserve.
The occurrence of low or insufficient oocyte production is relatively common. The condition affects one in 1,000 women between the ages of 15 and 29 and one in 100 women between the ages of 30 and 39. On the other hand, ovarian decline occurs in nearly a quarter of patients undergoing IVF treatment and is inevitable with ovarian aging in the later reproductive years.
Because of this, reproductive science has directed its attention to the core causes of these symptoms, and ovarian rejuvenation is one of the most promising treatments which has emerged. It works by affecting the dormant eggs in a woman’s ovaries, eggs with which all women are born and that are released by various quantities. When mature, the eggs travel down the fallopian tube to the uterus for fertilization. As we age, however, the number of eggs released tends naturally to decrease as well as the hormones produced to stimulate them.
Step by Step - How is ovarian rejuvenation done
The SEGOVA Program offers three therapy levels—PRP-based, stem cell-based, and tissue-based —designed to restore ovarian function and enhance fertility based on individual patient needs.
Want more details on all therapy levels?
Growth factor Platelet-Rich Plasma (PRP therapy) is the first level and part of the rejuvenation process. PRP Ovarian treatment – breaks down into five main phases or steps.
- Step 1: A sufficient amount of blood is taken from the patient’s forearm. The amount is determined by the general health of the patient, levels of hemoglobin, and other factors taken from a blood panel. This blood is needed to be subsequently used to stimulate the growth of new and existing eggs and restore hormonal balance;
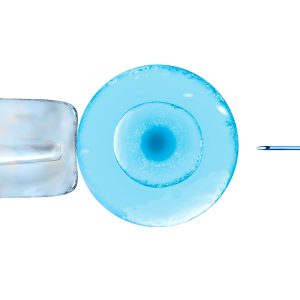
- Step 2: The drawn blood is then spun in a centrifuge to separate the red blood cells to obtain platelet-rich plasma (PRP). The process is called “autologous,” or deriving from the patient’s own body. This eliminates any risks of incompatibility;
- Step 3: The PRP is then tested in the laboratory and subjected to further purification and preparation for the patient’s ovary. Our teams employ sophisticated technology and take sufficient care to make sure that the PRP is prepared in an optimum way;
- Step 4: The treated and purified PRP is re-injected into the patient’s ovary in a minimally invasive procedure. The PRP, as we will see later, is meant to act as an agent for activating ovarian stem cells and causing them to generate new eggs.
- Step 5: Once the procedure has been completed, the growth of follicles is closely monitored and a standard course of IVF treatments are followed for the next six months.
The overall effect of ovarian rejuvenation comes with the activation of stem cells in the ovaries, assisting in the production of new eggs and follicles, either naturally or helped with IVF stimulation hormones. Moreover, the PRP injection has the effect of bolstering the hormonal functions of the ovary and, it is hoped, the chances of successful pregnancies.
This is a basic overview of how ovarian rejuvenation can look.
What is Platelet-Rich Plasma?
Platelet-Rich Plasma, or PRP, is central to the concept of ovarian rejuvenation and increasing the fertility rate in women with low or low-quality egg production for any of many possible reasons.
Platelets are blood cells and may be considered as natural healing vehicles. Our platelets promote blood clotting as a reaction to cuts on the skin. Our platelets also contain proteins in the blood that help wounds and damaged tissues to heal.
By injecting areas of inflammation or tissue damage with high concentrations of platelets, it encourages the restoration of healthy cells.
Blood drawn from the patient is put into a centrifuge, spun at high speeds, and this process separates platelets from all other blood elements. The platelets are then injected into the area to be treated as a kind of concentrated infusion of the blood’s most healing properties.
The platelet mixture, being several times more concentrated than naturally occurring in blood that has not been centrifuged, has been shown to dramatically increase healing.
PRP injections have been used in several different therapeutic areas to speed up the action of cells either for healing or repair.
It has been used to good effect for tissue healing and following plastic surgery to cut down the healing time and inflammation associated with it. Moreover, it has been successfully used for athletes to treat injuries in muscles, tendons, and ligaments.
PRP has been seen to have a salutatory effect on inflammation, and doctors have used PRP to reduce inflammation caused, for instance, by osteoarthritis. The treatment is meant to reduce pain and stiffness in joints.
PRP therapy has shown remarkable success in helping patients for fertility issues as in the ovarian rejuvenation process under discussion here.
The Stem cell therapy – second level of ovarian rejuvenation procedure
There are other and more advanced methods and practices, however, that go beyond this basic level. Some work to ensure even better results by the introduction of stem cells, or undifferentiated cells that may develop into distinct and specific cells and reproduce themselves, from the patient’s own body. These may be taken, as in the case of SEGOVA Biotechnology, from the pelvic bone, for example. Stem cell research has advanced greatly in the past decade and its application in ovarian rejuvenation is only one example of this phenomenal process.
Stem cell therapy, the first part of the process, has made tremendous strides from the early days of its research. Today, doctors use what are called “autologous stem cells,” meaning cells coming from the patient herself.
This is done by extracting bone marrow from the patient’s tibia, the shinbone, or pelvic bone under general anesthesia.
After the extraction, bone marrow is aspirated and centrifuged in sterile conditions, and three layers are obtained: acellular portion (platelet-poor plasma), red blood cells and bone marrow aspirate concentrate (BMAC) with nucleated cells. The obtained BMAC with stem cells is diluted with platelet-poor plasma and further used for treatment.
The use of mesenchymal bone marrow stem cells is done in order to stimulate the natural capacity of the gonadal tissue (the ovaries) to produce new follicles and eggs. The stem cells, prepared and transplanted, revitalize the ovary to produce new eggs. This is done to generate new non-differentiated gonadal stem cells, and these are to be developed into new oocytes and hormone-producing cells. The process may also incite existing gonadal stem cells to become activated.
Another effect of stem cell therapy is the improved functioning of hormones in the ovaries. The eggs do not produce hormones but rather the hormones come from the cells around them. The transplanted stem cells work to restore and regulate the endocrine function in hormone-secreting cells.
Mitochondrial boosting
While stem cell therapy happens in the lab, energy mitochondrial boosting is a recommended exercise regime employed to help slow down aging at the cellular level by increasing the production of mitochondria, your cells’ energy-releasing powerhouses, but also to restore endocrine balance. Practicing HIIT (High-Intensity Interval Training), a woman may boost her own mitochondrial energy production. HIIT is a cocktail of high intensity, isochronous, and very specific anaerobic exercises.
Third level of ovarian rejuvenation - Ovarian in Vitro Activation
It is autologous genetic treatment, or genetic treatment from the patient’s own body, of the gonadal tissue to restore and repair the ovary’s reproductive and endocrine functions. The activation is carried out in vitro and then the tissue is reintroduced into the ovary, rejuvenating and reactivating hormones and egg production.
What is SEGOVA Method?
SEGOVA stands for:
This unique, multi-level approach combines autologous stem cells, advanced plasma therapies, tissue activation, and metabolic optimization. SEGOVA is designed to reactivate ovarian stem cells, promote new follicle growth, restore hormonal balance, and increase the chances of natural conception or IVF success.
SEGOVA is regarded as the most advanced, the most innovative and safest means of achieving true ovarian rejuvenation because the method applies its extensive scientific and medical research in the service of the natural processes and functions of the patient’s body – ovaries, blood, and stem cells.
The SEGOVA method, therefore, introduces more precision into the process of ovarian rejuvenation, and therefore a higher chance of success in treating fertility issues in women who need it. Another benefit is that the repair of the hormonal systems will also improve the general health and well-being of patients.
What is Dual SEGOVA Method?
Dual SEGOVA (DOS – Dual Ovarian Stem Cell Therapy) is an absolutely unique, most cutting-edge ovarian rejuvenation program, devised by Professor Aleksandar Ljubić and his team. In Dual SEGOVA, we simultaneously utilize two types of autologous stem cells (SC) – mesenchymal and hematopoietic. These cells are extracted from bone marrow (mesenchymal and hematopoietic) and sometimes peripheral blood (predominantly hematopoietic). Their abilities to differentiate, modulate the immune response, and stimulate angiogenesis make them powerful tools in regenerative reproductive medicine.
The key principle of Dual SEGOVA is the concurrent application of mesenchymal and hematopoietic stem cells, which synergistically enhance each other’s effects. This approach allows for the collection of a significantly larger number of stem cells, with the possibility of cryopreservation for future use, thereby improving the overall outcomes of the therapy.
These two types of stem cells are used in conjunction with biological scaffolds, bioregenerative fibrine derived from the patient’s own blood to ensure local retention and enhance the desired effects. Additionally, growth factors from PRP and tissue activation in vitro are applied to further optimize the therapy.
By restoring ovarian function, DOS therapy can improve fertility, but also positively affect a woman’s overall health, including heart, bone, and mental well-being. The effects of DOS therapy are reflected in the improvement of natural ovarian hormone production in the vast majority of patients, lasting for several years. In half of the postmenopausal patients, menstruation returns.
What are the results?
What is the hormonal success rate of ovarian rejuvenation?
In order to accurately gauge the results, aside from happily pregnant patients which comes later on in the process, we turn first to the biochemistry and look at the different hormone levels and their activity on a regular basis. The increase or decline of hormonal production is key in determining how the ovarian rejuvenation process has worked.
Four major hormones are examined. Follicle-stimulating hormone (FSH) is the first hormone to be measured. FSH is an important part of the reproductive system. It is responsible for the growth of ovarian follicles. Follicles produce estrogen and progesterone in the ovaries and help maintain the menstrual cycles; Secondly, we look at the luteinizing hormone (LH). This is a hormone produced by gonadotropic cells. In females, when there is a spike in LH, it triggers ovulation; We then look at E2, estradiol, as a form of the hormone estrogen, and finally – Progesterone (PG), the female hormone that regulates the menstrual cycle and is crucial for pregnancy. The FSH, LH, E2, and PG levels are measured at regular intervals over a period of six months while the regular IVF treatment is in progress. If the FSH and LH levels become lower and the estradiol levels go up, it shows evidence of ovarian rejuvenation.
In results with 73 women, tested at three months, six months, and one year showed that after 6 months, FSH levels fell significantly. With the 25.8% drop in FSH, LH also dropped by 25% during the same period, although it was already visible after three months after the procedure.
E2 levels already grew from the 3-month mark by 26,6%. Meanwhile, progesterone levels were reduced during the period of one year following the procedure.
The overall results on this small group indicate clear benefits to the SEGOVA procedure and the creation of highly favorable conditions for increased fertility
What is the reproductive success rate of ovarian rejuvenation?
Many women see significant improvements in ovarian function and fertility after SEGOVA rejuvenation.
See detailed success rates and clinical results.
What is the age limit for ovarian rejuvenation?
There is no fixed chronological limit — what matters is your biological ovarian age.
We have successfully treated women aged 25 to 63 years, provided ovarian volume is adequate and menopause onset was less than 5 years ago. Learn more about eligibility.
Can I rejuvenate my ovaries naturally?
Yes! A holistic approach including proper nutrition, hormonal balance, exercise, stress management, and targeted supplements can support natural follicle growth and reproductive health. Read more here.
Are there any side effects to ovarian rejuvenation?
What are the potential risks or side effects of ovarian rejuvenation and the SEGOVA method? Evidence suggests that there are very few side effects and none serious enough to warrant deeper investigation. Using only your own cells and tissues, the SEGOVA method is among the safest procedures in reproductive medicine.
As injecting PRP and bone marrow stem cells, the main action of the procedure involves using a person’s own cells, they do not usually experience any adverse reactions to the injections.
Some potential effects, however, are still possible. So far, in 253 patients who underwent SEGOVA ovarian rejuvenation, in 5 cases adverse reactions were observed following the procedure. These include one case of PID (Pelvic inflammatory disease) which occurred three months after SEGOVA therapy and another case of muscle weakness in the brachialis (upper arm) after the procedure. There were also local reactions in the lower leg where the bone marrow has been extracted in three patients out of 73.
Although it is not a side effect, it must be born in mind that there can be no guarantee that a woman will conceive naturally or assisted by IVF techniques following such a procedure, even if it has been seen to increase the likelihood.
In a small number of women (around 20%), they will have some mild lower abdomen discomfort, perhaps sense pressure on the ovaries. There may even be a small amount of bleeding. However, these symptoms have also been seen to subside in the hours following the procedure in nearly all cases.
How long does the effect of ovarian rejuvenation last?
Preparation takes a few days, with 2–3 days in clinic.
First improvements may appear within 1–2 months, and results can last several years. Learn more about the process.
What is the cost of ovarian rejuvenation?
SEGOVA offers three levels of treatment, depending on ovarian reserve and individual needs.
Are there success stories from women like me?
Yes!
Read inspiring stories from women who have undergone ovarian rejuvenation with SEGOVA.
Can SEGOVA help with low AMH?
Absolutely. Even with low AMH levels, SEGOVA aims to improve ovarian environment and reserve.
Learn about AMH and ovarian function:
More Information?
The topic of ovarian rejuvenation is much discussed today among doctors, researchers, scientists, as well as prospective mothers – candidates for the procedure – and their families. As such, more discoveries are being made and more information is being published constantly.
We urge you to keep reading here to stay up to date with all of the advances in this exciting field that could affect you and your future family directly.
If you have questions, comments, or would like to know more about any part of ovarian rejuvenation, SEGOVA, or other related topics, please contact us here. Our doctors are standing by and ready to discuss all of your needs and concerns.
Ready to take the next step? Book your personalized consultation today and our medical team will guide you through the individual assessment and recommend the best treatment path for you.
This program is dedicated to all women seeking not only to improve their fertility but also to extend their healthy, active life. SEGOVA is more than a treatment — it is a vision of future reproductive health.