Published in Human Reproduction
Abstract
Study question
Does autologous bone marrow derived stem cell (BMDSC) ovarian transplantation optimize ovarian reserve parameters in young infertile women with diminished ovarian reserve (DOR) ?
Summary answer
The autologous stem cell ovarian transplantation (ASCOT) improves AFC and AMH by facilitating the recruitment of existing dormant follicles in young women with DOR.
What is known already
Oocyte donation is the practical therapeutic option when patients with premature ovarian ageing desire pregnancy. It involves significant psychological burden in terms of not able to have their own biological child. Ovarian rejuvenation has opened new doors in poor responders and premature ovarian insufficiency through its beneficial effects on ovarian reserve and IVF outcomes. However recent studies have shown contradictory results in terms of its efficacy. No prior study has been contemplated in DOR group
Study design, size, duration
An open label non randomized controlled trial was conducted at Division of Reproductive Medicine in collaboration with stem cell facility at tertiary care institute. Forty two infertile women less than 35 years age with DOR (AFC<5, AMH<1.2ng/ml and /or high FSH>8IU/l) were enrolled in the study during a period from January 2020 to December 2020. 20 women who did not opt for the intervention were treated as control group whereas 22 women received the intervention.
Participants/materials, setting, methods
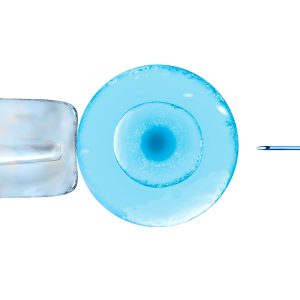
Baseline hormonal profile ( Day 2 FSH, estradiol, AMH and AFC) was done in all patients. Women with abnormal uterine cavity, endometriosis, prior ovarian surgery, abnormal karyotype were excluded. Bone marrow aspiration followed by mesenchymal stem cells isolation was performed. The stem cells were transplanted in both the ovaries through transvaginal route on the same day. Follow up visits were planned at one and six months to assess ovarian reserve parameters.
Main results and the role of chance
The mean age, BMI and duration of infertility were comparable between the control and study group (29.5±3.34vs 29.36±2.95years, 21.51±1.40vs21.87±1.93kg/m2, 6.9±1.94vs7.04±3.67 years). The positive response in terms of improved AMH and AFC was seen in 68% (15/22) patients. The mean number of stem cells injected in these women were 77.71±25.33 million. At first follow up, there was no significant difference between mean FSH, estradiol levels and mean right and left ovarian volume (9.23±3.95 vs 9.02±3.92mIU/l, 61.46±29.25 vs 68.12±62.52 pg/ml, 2.82±2.18 vs 2.44±1.25 cc, 2.02±1.54 vs 2.72±1.06 cc, p < 0.05). There was significant increase in AMH and AFC values as compared to baseline (0.79±0.43 vs 1.26±0.82ng/ml, p = 0.03; 3.47±1.30 vs 6.40±2.23, p < 0.001). At second follow up visit, the significant increase in ovarian reserve persisted for AMH and AFC (0.79±0.43 vs 1.22±0.76 ng/ml, p = 0.02; 3.47±1.30 vs 6.93±1.71,p<0.001). There was no significant difference between serum FSH, Estradiol and ovarian volume. None of the patients developed any complication and the improvement in AFC and AMH persisted during 10 month follow up period.
Limitations, reasons for caution
The limitation of present study is small sample size and non randomization. However, time period for which positive effect lasts has not been documented in earlier studies. This study is currently being endeavored, and women with improved ovarian reserve are followed up for any spontaneous conception or following assisted reproduction.
Wider implications of the findings
The present study demonstrates beneficial role of stem cells in improving ovarian reserve parameters in women with DOR with no acquired cause. If supported by future randomized clinical studies, it could represent a paradigm shift for fertility treatment in these women providing an opportunity to have their own biological child
Read more at https://academic.oup.com/humrep/article/36/Supplement_1/deab128.037/6343686