Published in Journal of Human Reproductive Sciences
Abstract
Background:
The management of poor responders is still a challenge in modern-assisted reproductive technology. Several researches show encouraging results with individual autologous bone marrow-derived stem cells (ABMDSCs) and platelet-rich plasma (PRP). Hence, we decided to study the synergistic effect of ABMDSCs with PRP.
Aims and Objective:
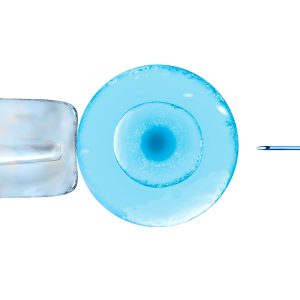
The aim of the study was to assess the safety and efficacy of intraovarian instillation of ABMDSCs combined with PRP in poor responders.
Design:
This was an interventional pilot study. Study Period: January 2017 to January 2019.
Materials and Methods:
We designed a pilot study using Patient-oriented Strategies Encompassing IndividualizeD Oocyte Number (POSEIDON) Group 3 and 4 poor responder patients (n = 20). The study group underwent laparoscopic/transvaginal intraovarian instillation of ABMDSCs combined with PRP and the outcome was analyzed – primary outcome – antral follicular count (AFC) and mature MII oocytes and secondary outcome – Anti-Mullerian hormone (AMH) levels and number of Grade A and B embryos frozen on day 3. The Wilcoxon signed-rank test and Pearson correlation were used for the statistical analysis and P < 0.05 was considered statistically significant.
Results:
After 6 weeks of intraovarian instillation ABMDSCs mixed with PRP, patients were reassessed for AFC and AMH and their response to subsequent controlled ovarian stimulation (COS) cycle was observed. Statistically, significant improvement was seen in AFC, MII oocytes, and Grade A and Grade B embryos. AMH was also increased in some patients, but the result was not statistically significant.
Conclusion:
Our results suggest that intraovarian instillation of ABMDSCs combined with PRP is safe, and it optimized the recruitment of existing dormant primordial follicles to improve oocyte yield and hence the number and quality of embryos after COS in POSEIDON Group 3 and 4 poor responders.
Read more at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7727891/