In modern regenerative gynecology, two biological therapies are particularly significant in efforts to revitalize ovarian function in women with diminished ovarian reserve: platelet-rich plasma (PRP) therapy and autologous stem cell therapy, including mesenchymal (MSC), hematopoietic (HSC), or a combination of both. The SEGOVA platform enables the implementation of each of these methods individually, as well as through an integrated “Dual SEGOVA” protocol that combines their advantages.
PRP Therapy – Specifics in Ovarian Rejuvenation
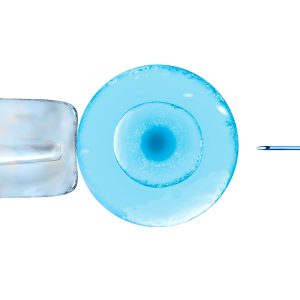
PRP (Platelet-Rich Plasma) therapy uses autologous plasma enriched with platelets, extracted from the patient’s peripheral blood. After centrifugation and concentration, the PRP is injected directly into the ovarian tissue.
Mechanism of action:
- Release of high concentrations of growth factors (VEGF, PDGF, IGF-1, TGF-β)
- Activation of local stem cells
- Improvement of microcirculation and regeneration of the ovarian stromal component
Clinical effects:
- Statistically significant increase in AFC (antral follicle count) after 3 months
- Increase in AMH and estradiol levels in some patients
- Return of menstruation in a portion of previously amenorrheic patients
- Rapid effect and excellent safety profile
Stem Cell Therapy – MSC, HSC, or Combined Application
Stem cells are most commonly obtained from the patient’s bone marrow (MSC and HSC) or adipose tissue (MSC). After isolation and processing (native or cultured), the cells are injected into the ovarian tissue.
Mesenchymal Stem Cells (MSC):
- Act paracrinally by releasing factors that promote tissue regeneration, angiogenesis, and immunosuppression
- Enhance cellular reactivity of the ovarian stromal tissue
Hematopoietic Stem Cells (HSC):
- Strong influence on immunohematologic functions of the ovarian microenvironment
- Contribute to vascular reorganization and repair of damaged niches
Clinical characteristics:
- Slower effect compared to PRP (requires 6–12 weeks for evaluation)
- Suitable for more severe insufficiency and early POF (premature ovarian failure)
- Potential for deeper regeneration of stromal and vascular components
Limitations:
- Higher technical requirements
- Higher cost threshold
Integrated Approach – Dual SEGOVA
Dual SEGOVA combines the advantages of both therapies in a strictly personalized protocol:
- PRP therapy could be used as the initial biostimulant
- Based on response evaluation – MSC, HSC, or a combination
- Monitoring: Continous hormonal and ultrasound follow-up
- Possible additional phases: In vitro activation, metabolic and hormonal optimization
Advantages of integration:
- Rapid response from PRP combined with the deep regenerative potential of stem cells
- Flexibility of the therapeutic plan depending on response and goals (e.g., natural ovulation, IVF preparation)
- Maximized use of autologous potential without the use of hormones
Conclusion
PRP and stem cell therapies are not competing, but complementary methods in modern treatment of ovarian dysfunction. PRP is a simple, fast, and safe tool for initiating regeneration, while MSC and HSC enable deeper restoration in more complex cases. Through the Dual SEGOVA approach, the highest level of personalized regenerative strategy can be achieved, based on objective monitoring of biological response and ovarian function recovery.