Beyond AMH — What Else Indicates Ovarian Reserve?
More and more women today are choosing to start families later in life. With this shift, there’s a growing need for early and accurate ways to assess ovarian function. Understanding ovarian reserve is essential for planning ahead — whether it’s for fertility preservation, reproductive treatments, or overall health.
While AMH (Anti-Müllerian Hormone) is often considered the go-to marker, it’s not the only one. A full evaluation of ovarian health involves looking at several important indicators. Let’s break down what they are, and why they matter.
Why Is Ovarian Function Assessment Important?
The ovaries are responsible for two key roles:
· Producing and maturing eggs
· Secreting hormones that support reproductive and overall health
As ovarian reserve naturally declines with age, assessing it helps with:
· Planning when and how to start a family
· Deciding whether fertility preservation (like egg freezing) is needed
· Supporting long-term health, since reproductive hormones affect bones, heart, metabolism, and more
Most Common Markers of Ovarian Reserve
Anti-Müllerian Hormone (AMH)
Often seen as the “gold standard,” AMH is produced by small follicles in the ovaries. It gives a snapshot of how many potential eggs a woman still has.
· High AMH: Suggests a strong egg reserve, but may also be seen in women with polycystic ovary syndrome (PCOS)
· Low AMH: Suggests reduced ovarian reserve and may signal challenges with natural conception
FSH (Follicle-Stimulating Hormone)
This hormone is produced by the pituitary gland and plays a crucial role in egg development. It’s typically measured on day 2 or 3 of the menstrual cycle.
· High FSH (usually >10 IU/L): May indicate low ovarian reserve. The body needs to produce more FSH to stimulate follicles when reserve is low
· Low to normal FSH: Generally reflects better ovarian function, but should always be interpreted along with other markers
Estradiol (E2)
Estradiol is the main female sex hormone, and like FSH, it’s measured early in the cycle.
· High early-cycle estradiol can make FSH levels seem normal, masking a potential issue
· Low to moderate E2: Typically a good sign of ovarian health
Inhibin B
Though less commonly discussed, Inhibin B is also secreted by ovarian follicles.
· Low Inhibin B: May indicate declining follicle quantity and reduced ovarian reserve
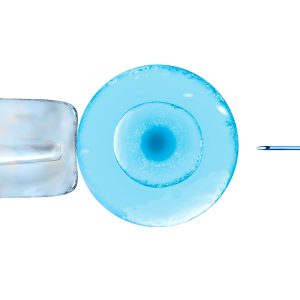
Antral Follicle Count (AFC) and Ultrasound
A transvaginal ultrasound allows doctors to count antral follicles — small follicles 2 to 10 mm in size — at the beginning of the cycle.
· More antral follicles: Suggests a higher egg reserve
· Ovarian volume and structure: Can reveal additional concerns like cysts or polycystic ovaries
Clomiphene Citrate Challenge Test (CCCT)
While not as common today due to AMH testing, this test can still be useful. It involves:
1. Measuring FSH on day 2
2. Taking clomiphene citrate (days 5–9)
3. Measuring FSH again on day 10
· Elevated FSH after medication: Indicates a lower ovarian reserve and weaker ovarian response
Why Should These Markers Be Viewed Together?
No two women have the same hormonal profile. Looking at just one number — AMH, FSH, or estradiol — may not tell the whole story.
For example:
· High estradiol might falsely suppress FSH, making it seem normal
· High AMH might not always mean good fertility — in PCOS, AMH levels are often unusually high
This is why fertility specialists recommend a comprehensive hormone panel (AMH, FSH, estradiol, LH, Inhibin B) alongside an ultrasound scan.
Only by considering all of these markers together can you get a clear, accurate picture of your ovarian reserve — and take the right steps for your future fertility and health.