For women with diminished ovarian reserve (DOR), IVF can be one of the biggest challenges. Traditional protocols often yield disappointing results, making it essential to explore newer, more advanced approaches.
The good news? Innovative treatments like biological IVF, ovarian PRP therapy, stem cell rejuvenation, and in vitro ovarian activation (IVA) are giving hope to women with low ovarian reserves.
Let’s break down the best strategies for improving IVF success when ovarian reserve is low.
Assessing Ovarian Reserve
Before selecting an IVF protocol or regenerative therapy, it is crucial to assess ovarian reserve using the following tests:
- AMH (Anti-Müllerian Hormone) – A marker of the remaining follicle count.
- Antral Follicle Count (AFC) – Ultrasound evaluation of the number of small follicles.
- FSH and Estradiol (E2) at the start of the cycle – High FSH indicates diminished reserve.
- Inhibin B – An additional marker of ovarian function.
These parameters help tailor the stimulation protocol or regenerative treatment.
IVF Protocols for Patients with diminished ovarian reserve
1. Modified Long Agonist Protocol
This protocol uses low doses of GnRH agonists (buserelin, leuprolide) to achieve mild pituitary suppression before gonadotropin stimulation.
✔ May improve follicular recruitment in certain patients
✔ Reduces the risk of premature LH surge
❌ May cause excessive suppression in patients with already low ovarian reserve
2. Antagonist Protocol (Short Protocol)
The most commonly used protocol for patients with diminished reserve. GnRH antagonists (cetrorelix, ganirelix) are introduced when follicles reach 12-14 mm to prevent premature LH surge.
✔ Flexible and shorter cycle
✔ Less pituitary suppression and potentially better follicular response
✔ Lower risk of ovarian hyperstimulation syndrome (OHSS)
❌ May result in fewer oocytes compared to long protocols
3. Mild Stimulation Protocol
Uses low doses of gonadotropins (75-150 IU) or a combination with letrozole to achieve controlled stimulation without excessive ovarian suppression.
✔ May improve oocyte quality
✔ Lower risk of complications
✔ Reduced need for high hormone doses
❌ Usually yields fewer oocytes
4. Natural IVF and Modified Natural IVF
This strategy utilizes the patient’s natural cycle with little or no stimulation.
✔ Ideal for patients who prefer minimal hormonal stimulation
✔ Lower costs and fewer side effects
❌ Very few oocytes obtained per cycle
5. Double Stimulation (DuoStim / Shanghai Protocol)
Involves two ovarian stimulations in the same cycle—one in the follicular phase and one in the luteal phase.
✔ Allows retrieval of more oocytes in a shorter period
✔ Especially beneficial for patients experiencing rapid ovarian function decline
❌ Can be physically demanding due to intense hormonal stimulation
Regenerative Therapies and Biological IVF Approaches
1. Biological IVF with Ovarian PRP Therapy
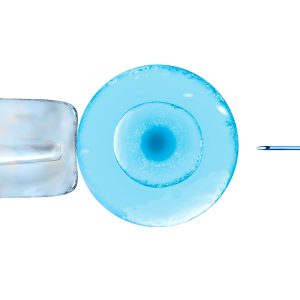
Biological IVF combines a natural or mild stimulation cycle with ovarian PRP therapy, where autologous platelet-rich plasma is injected directly into the ovaries to enhance the function of remaining follicles.
✔ May improve ovarian response in women with low AMH
✔ Safe and easy to perform
2. Ovarian Rejuvenation with Stem Cells
Ovarian Rejuvenation with Stem Cells utilizes autologous stem cells (MSC and HSC) to stimulate ovarian regeneration.
- Single-type stem cell therapy uses stem cells (SC) derived from bone marrow, adipose tissue, or peripheral blood.
- Dual stem cell therapy (MSC + HSC) combines mesenchymal (MSC) and hematopoietic stem cells (HSC) to optimize tissue regeneration and improve ovarian vascularization.
✔ MSC release paracrine factors that may increase the number of antral follicles
✔ HSC improve angiogenesis and ovarian microcirculation
❌ The therapy is still experimental and not widely available
3. In Vitro Activation of Ovarian Tissue (OVA)
OVA involves extracting ovarian tissue, activating it in vitro, and reimplanting it into the patient to stimulate the growth of “dormant” follicles.
✔ May stimulate the growth of remaining inactive follicles
✔ Applicable for women with primary ovarian insufficiency (POI)
❌ The procedure is invasive and available only in specialized centers
Conclusion
There is no universal protocol for patients with diminished ovarian reserve. A personalized approach is key—combining the optimal stimulation protocol with regenerative therapies can significantly improve pregnancy chances for women with low ovarian reserves.
🔹 Mild IVF and PRP therapy – for women with moderately diminished reserve
🔹 MSC + HSC therapy – for women with severely diminished reserve
🔹 IVA method – for patients with primary ovarian insufficiency
If you have experience with these protocols or regenerative therapies, share your thoughts in the comments!