Stem cell therapy (with stem cells obtained from the patient’s own body) aims to create new or incite existing non-differentiated ovarian stem cells – which are to be developed into new egg cells and hormone-producing cells.
The ‘no new eggs’ doctrine has a long history. In 1951, the influential anatomist Solly Zuckerman, at the University of Birmingham, UK, performed an in-depth analysis of evidence available at the time. He concluded that female mammals stop producing oocytes after birth. It was from this limited “bank account” of egg cells, the understanding went, that a woman would “draw down” with each ovulation, and from which she would also lose viable eggs due to genetic and other ageing damage. When her egg cell “bank balance” fell below some limit, the loss of crosstalk amongst egg cells, follicles, and the regulatory centres in the brain would cause her follicles to atrophy and stop producing estrogen, leading to the symptoms of menopause.
However, recent studies are showing that female germline stem cells still exist in mammalian ovaries after birth. In 2004, animal studies showed that the ovaries possess rare female germ line or oogonial stem cells (OSCs), which could generate oocytes and off-springs. Moreover, cases were being reported of women who had regained their fertility after having had it destroyed by cancer therapy: months or years after being rendered infertile and suffering from menopausal symptoms, women who had received bone marrow transplants would spontaneously begin cycling again, with several cases of spontaneous pregnancies reported.
Where were the eggs coming from? There were two possibilities. One was that factors in the bone marrow transplants were contributing growth factors and other molecules that were resuscitating follicles that had been inactivated by the chemotherapy, allowing them to release a supply of egg cells that were secretly lying dormant within them. The other, even more, exciting possibility: the transplanted cells were coming into the follicles and regenerating their capacity to produce completely new egg cells. The OSC lie dormant in aging women, waiting to be revitalized with the right cocktail of cells or signalling factors. This would be expected to extend reproductive lifespan and postpone or reverse menopausal symptoms, so long as the body could continue to generate new OSC.
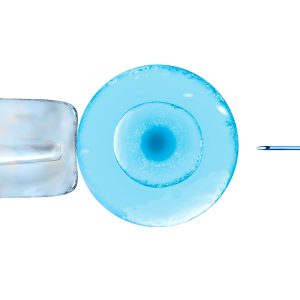
Stem cells are undifferentiated cells with unlimited capacity to divide. Within our bodies we have sources of stem cells which can further develop in any given cell type. Bone marrow stem cells are used for ovarian rejuvenation. Stem cell therapy has contributed greatly to regenerative medicine and it is used in orthopaedics, cardiovascular medicine, dentistry, maxillofacial, plastic and esthetic surgery and other medical branches. Anti-ageing is the biggest field of research for a stem cell application, and in our case it is significant for fertility treatments. This treatment aims to create new eggs using the intrinsic capacity of the ovarian tissue. Injecting bone marrow stem cells into the ovary stimulates follicles and egg growth. This growth can be caused by the factors present in the bone marrow which activate and assist growth factors and other molecules inside the ovarian tissue. Another possibility is that transplanted cells restore the capacity of the ovarian tissue to produce completely new eggs.
Stem cell technology leads to improved ovarian hormone function. Hormones are not produced by the eggs, but by the surrounding cells. Growth factors and other factors induced by the SCOR technology increase the activity of these cells and increase the level of hormones produced by the ovary. Application of SCOR technology has significant advantages compared to hormone replacement therapy – HRT, which has been the base treatment for postmenopausal women for decades. Although HRT alleviates unpleasant menopausal symptoms and decreases bone mass loss, it can increase the risk of stroke and some cancers. Ovarian rejuvenation and revitalization restores ovarian hormone function under natural body regulation mechanisms and doesn’t have dangerous side effects.
Mesenchymal bone marrow stem cells are used for gonadal rejuvenation. This treatment aims to create new eggs using the intrinsic capacity of the gonadal tissue. Injecting bone marrow stem cells into the ovary stimulates follicles and egg growth. Transplanted stem cells restore the capacity of the ovarian tissue to produce completely new eggs.
Stem cell technology also leads to improved ovarian hormone function. Hormones are not produced by the eggs, but by the surrounding cells. Growth factors and other factors induced by the Stem cells increase the activity of these cells and increase the level of hormones produced by the ovary.
However, a major difficulty with stem cell therapy is to maintain cell viability, properties and function of stem cell before and after implantation in vivo. Once stem cells are isolated from the native tissue environment, they quickly lose the niche and function they had when growing in culture dishes. In addition, they shorten cell lifespan because of over-expansion in vitro. Furthermore, cellular DNA tends to be unstable during long-term culture. Such cells implanted in the host lead low rates of cell survival, and poor outcomes in-growth, homing, differentiation and paracrine effects.
SEGOVA program overcomes these problems by offering autologous stem cell therapy without the incubation.