Results of Ovarian Biological Therapies
The most reliable studies in the field of medicine are systematic reviews and meta-analyses, which form the foundation for medical protocols. Here, we present systematic reviews of all published studies that have investigated therapies using PRP growth factors, in vitro tissue activation, and stem cells for ovarian function decline. Additionally, we share the results of the SEGOVA and Dual SEGOVA – Dual Stem Cell Ovarian Activation (DSA) therapies.
These findings were presented by Academician Aleksandar Ljubić at the International Congress on Reproduction, organized by the Middle East Fertility Society (MEFS) in Doha, Qatar, in November 2024.
Biological Reproductive Therapies
Biological reproductive therapies are advanced treatments utilizing cells, such as stem cells, and their biologically active products to regenerate and enhance ovarian and reproductive system function.
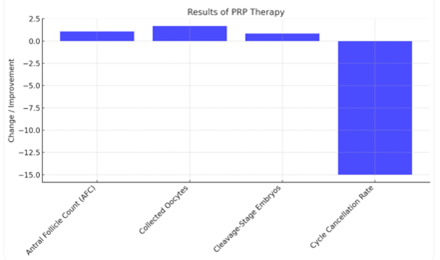
Platelet-Rich Plasma (PRP) Therapy
- Findings from Systematic Review:
- Women with diminished ovarian reserve (DOR) showed significant improvements:
- Antral follicle count (AFC): Increase of 1.07.
- Collected oocytes: Increase of 1.68.
- Cleavage-stage embryos: Increase of 0.85.
- Cycle cancellation rate: Decrease by 15%.
- Women with diminished ovarian reserve (DOR) showed significant improvements:
- Study Scope:
- 14 studies involving 1,632 participants.
- The first systematic analysis of PRP therapy effects on human subjects (1).
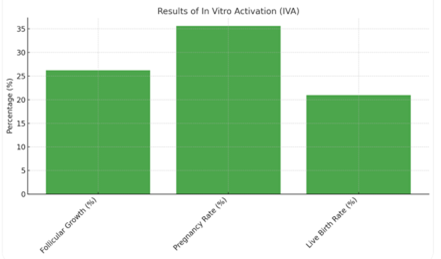
In Vitro Activation (IVA) of Ovarian Tissue
- Findings from Systematic Review:
- Follicular growth observed: 26.21% in patients with premature ovarian insufficiency (POI).
- Pregnancy rate: 35.58% (11 pregnancies out of 43 participants with follicles).
- Live birth rate: 20.93% (9 live births).
- Meta-Analysis of Cryopreservation:
- 26 pregnancies (14.68%) and 18 live births (10.16%) achieved from cryopreserved ovarian tissue.
Conclusion:
IVA shows promise for fertility preservation, particularly in younger patients with residual ovarian follicles. Experimental drug-free activation techniques demonstrate higher efficacy but require further standardization and safety evaluation.
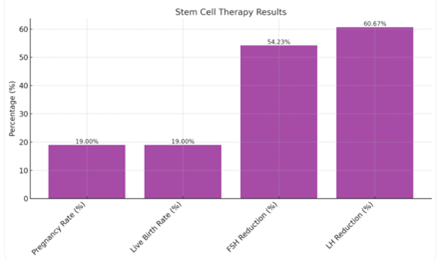
Stem Cell Therapy
- Animal Studies:
- 37 studies involving 1,079 animals (rats, mice, rabbits).
- Hormonal Improvements:
- Estradiol (E2): Significant increase (SMD 2.69).
- FSH: Significant decrease (SMD -2.02).
- Follicle regeneration showed statistically significant increases in primary, secondary, and primordial follicles.
- Clinical Results:
- Analysis of 21 human clinical studies (~900 participants).
- Fertility Improvements:
- Pregnancy rate: RD 0.19.
- Live birth rate: RD 0.19.
- Safety: No significant adverse effects reported.
- Stem Cell Sources:
- Stem cells from umbilical cord (UC-MSCs) and bone marrow (BM-MSCs), administered intravenously and intra-ovarian, allogeneic and autologous.
OUR results
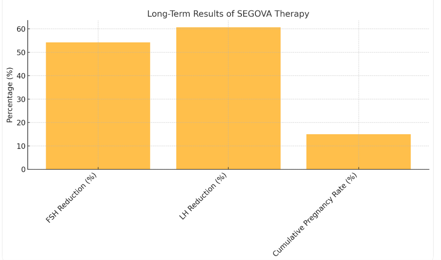
Combination of PRP, In Vitro Activation, and Stem Cells (SEGOVA)
- SEGOVA – Long-Term Data (7-Year Cumulative Analysis, 73 Patients):
- Hormonal improvement in 85% of patients.
- FSH reduction: Noticeable after 6 months, with a maximum decrease of 54.23% at 24 months.
- LH reduction: Decline after 6 months, reaching 60.67% at 24 months.
- Cumulative pregnancy rate: 15%.
- Dual Ovarian Stem cell Therapy (DOS):
- Combination of autologous PRP, IVA, BM-MSCs, and hematopoietic stem cells (HSCs) on a fibrin matrix, with cryopreservation.
- Preliminary results indicate a 20-25% improvement compared to conventional SEGOVA therapies.
Conclusion
These systematic reviews represent the first comprehensive analyses conducted on human subjects, emphasizing the need for further large-scale studies to optimize these therapies for clinical application.
The combined application of PRP, IVA, and stem cell therapies demonstrates synergistic potential for ovarian regeneration. These methods, including Dual Ovarian Stem Cell Therapy, represent the pinnacle of contemporary approaches for restoring ovarian function.
REFERENCES
1. Maged, A. M., Mohsen, R. A., Salah, N., & Ragab, W. S. (2024). The value of intraovarian autologous platelet rich plasma in women with poor ovarian reserve or ovarian insufficiency: a systematic review and meta-analysis. BMC pregnancy and childbirth, 24(1), 85. https://doi.org/10.1186/s12884-024-06251-2
2. Escarcega-Bordagaray, J. A., Torres-Martinez, M., Hinojosa-Gonzalez, D. E., Ramírez-Díaz, M., Fàbregues, F., & Carmona, F. (2024). Basal characteristics of patients who responded to Ovarian Fragmentation for Follicular Activation (OFFA) or In Vitro Activation (IVA): a systematic review and meta-analysis. Journal of assisted reproduction and genetics, 41(4), 989–998. https://doi.org/10.1007/s10815-024-03046-4
3. Wang, W., Todorov, P., Isachenko, E., Rahimi, G., Mallmann, P., Wang, M., & Isachenko, V. (2021). In vitro activation of cryopreserved ovarian tissue: A single-arm meta-analysis and systematic review. European journal of obstetrics, gynecology, and reproductive biology, 258, 258–264. https://doi.org/10.1016/j.ejogrb.2021.01.014
4. Hu, L., Tan, R., He, Y., Wang, H., Pu, D., & Wu, J. (2024). Stem cell therapy for premature ovarian insufficiency: a systematic review and meta-analysis of animal and clinical studies. Archives of gynecology and obstetrics, 309(2), 457–467. https://doi.org/10.1007/s00404-023-07062-0
5. Guo, C., Ma, Y., Situ, Y., Liu, L., Luo, G., Li, H., Ma, W., Sun, L., Wang, W., Weng, Q., Wu, L., & Fan, D. (2023). Mesenchymal stem cells therapy improves ovarian function in premature ovarian failure: a systematic review and meta-analysis based on preclinical studies. Frontiers in endocrinology, 14, 1165574. https://doi.org/10.3389/fendo.2023.1165574
6. Ljubić, A., Dinić, M., Milić J., Svetlana Vujović (2024): Revolutionizing Ovarian Regeneration: The Promise and Perils of Dual-Double Stem Cell Therapy. Invest Gynecol Res Women’s Health. 5(2). IGRWH. 000606. 2024. DOI: 10.31031/IGRWH.2024.05.000606
